Grumman/Butkus Associates’ engineering team recently played a pivotal role in a once-in-a-lifetime project: Turning the shuttered Westlake Hospital in Melrose Park, IL, into a 430-bed COVID-19 surge response facility in less than a month.
“It was a job we’ll be talking about for our entire lives,” says G/BA Associate Joe Ficek, who led the plumbing and fire protection response. The G/BA team was tasked with investigating the site, creating a workable engineering design, and overseeing installation and commissioning of mechanical and plumbing/fire protection repairs and revisions — all at breakneck pace.
The firm worked under the direction of the U.S. Army Corps of Engineers, which had determined with Illinois and Chicago authorities in late March that several FEMA-funded COVID surge facilities could be needed in Chicagoland. Westlake, a 240,000-square-foot hospital in the western suburbs, was one of four such sites implemented this spring. The hospital had been closed since fall 2019.
G/BA provided mechanical, plumbing, and fire protection design, construction administration, and commissioning services. Other key members of the team included general contractor Bulley & Andrews; electrical engineer Dickerson Engineering; and Anderson Mikos Architects. Key trade contractors and vendors included Jamerson & Bauwens, Terry Plumbing, Great Lakes Plumbing and Heating, Air Design Systems, Omni Pumps, Synergy Mechanical Inc., and Honeywell.
Rapidly creating a facility for moderate to acute COVID patients in a building that had been vacant for months, and had been troubled before that, was a massive undertaking, according to G/BA Vice President John Villani. “We found an incredible amount of failed pieces of equipment. The facility must have been on an austerity budget for at least five years, with minimal maintenance, a run-to-failure philosophy, and very few major upgrades for a decade or more.”
Staff members worked long hours, including nights, weekends, and the Easter holiday, to accomplish the mission. In addition to Ficek and Villani, G/BA’s team included Principal-in-Charge Gerry Noorts; G/BA Associate and Project Manager Mason; mechanical engineers Kevin Vander Klay, Daiju Varghese, Kurt Matsen, Samuel Schmidt, Inna Gorelik, and Alex Sir; plumbing/FP engineer Sergio Cano; and CAD specialist Paul Wozniakowski. Among all the participating firms, about 200 on-site staff were required to complete the job.
Investigation
Finding and assessing existing equipment and distribution systems, without accurate documentation, was the first hurdle. Says Vander Klay, “We were given access to their ATG Web platform, and we just started digging for information. Drawings through the years had been scanned and loaded, but some were mislabeled, some were missing, and some were just wrong. Very few areas were properly documented.”
Villani adds, “There was a lot of walking around, going into every mechanical room, looking above ceiling tiles, figuring out what was actually there.”
The older “main” hospital, comprising the North and East wings, had equipment dating from the 1950s and 1960s. The newer West building was constructed in the 1980s.
Existing infrastructure for the “main” hospital included:
- A steam plant with three steam boilers, the newest of which was installed in 1967. Only one was operable when G/BA arrived. “We had major steam issues, major condensate problems; the plant was just limping along,” says Villani.
- A cooling plant with three decades-old chillers. Again, only one of the three was functional.
- A dozen air-handling units, distributed among basement, upper floor, and penthouse mechanical rooms.
- Associated pumps and related equipment.
The West building infrastructure, which was not connected with the main hospital’s systems, included:
- A high-temperature, high-pressure hot water system, operating at roughly 100 pounds of pressure and 270 degrees, including three boilers and a nitrogen-pressurization system. “This was a unique situation,” Villani recalls. “Their original plan was to make this their main plant and to decommission the older steam plant. But for various reasons, that did not happen.” One of the three boilers had been scrapped and was being used for parts; only one of the two remaining units was functioning.
- A two-chiller cooling plant, with only one unit operable when the project commenced.
- Two AHUs.
- Associated pumps and related equipment.
Says Villani, “It is not that large a facility, but to have two separate plants adds a lot of complexity, and to address the many failed pieces of equipment was an enormous effort.” Lack of a functional building automation system compounded the problem; the old pneumatic controls were a jumble of oil- and water-logged pneumatic lines and receiver controllers, referred to by Villani as “a historical graveyard of pneumatic equipment.”
HVAC Design
The design team was given about a week to devise a plan and create construction drawings. In addition to addressing heating and cooling plant issues, key objectives included maximizing patient beds; meeting targets for negative patient room pressurization; and providing robust medical gas infrastructure, assuming that abundant oxygen and many ventilators would be needed.
Because the new Westlake Alternative Care Facility would only receive COVID-19 patients who had been diagnosed elsewhere, the team did not have to design the triage and waiting rooms required for a walk-in hospital. Food service would be limited to meals brought to the site, negating the need for a functional kitchen. An existing pharmacy was cleaned up but not renovated.
Patient beds were squeezed into every possible area, including former operating and recovery rooms. “In one isolation room, we might put two or three beds,” says Mason. “In ICU areas where they had one bed, we might squeeze in two. The original count of beds was 225 or so, but we got it up to over 400 beds because we converted so many areas where you would not normally place patient rooms.”
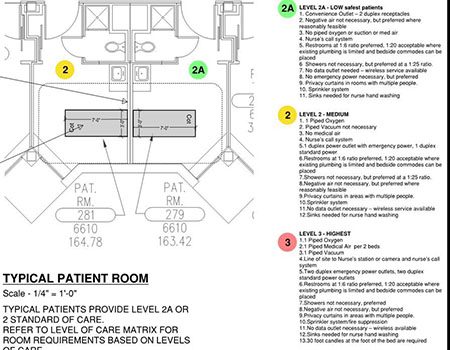
According to Mason, achieving pressurization goals was one of the toughest aspects of the design. “The original goal was to make the rooms achieve 0.01 inch negative pressure. But we soon reached the agreement that we only had to make the rooms negative if at all possible, because reaching 0.01 inch was not going to be possible in many of the oldest patient rooms. Our target value became 12 air changes per hour for exhaust and whatever supply we could get, but generally 100 cfm less than the exhaust. If we were exhausting 200 cfm, we were targeting 100 cfm for supply.” Ultimately, rooms intended to serve less-ill patients were allowed to meet less stringent pressurization goals.
Primary HVAC strategies included:
- Using the existing air supply and exhaust systems to achieve negative pressure where possible, including the 14 existing AHUs.
- Adapting rooms with supplemental equipment where the first tactic was not possible.
In some areas, goals were met by cranking all AHUs to supply 100% outside air at constant volume, and by repurposing toilet exhaust systems to provide (or increase) general room exhaust. Existing return exhaust grilles were pulled out of the ceiling and adjacent ductwork was cleaned; grilles were replaced with bird screening and converted to exhausts. Nurse station and support areas were oversupplied with supply air as much as possible, and this clean air cascaded down corridors and under patient room doors to help provide makeup air.
In the oldest part of the hospital, however, some rooms had no outside air supply available. Instead, they had double-hung, operable windows and were heated and cooled with wall-mounted fan coil units. These units were refurbished as needed, and for rooms that had toilet exhaust, the fans were cranked up as much as possible. Two small, new 100% outside air AHUs were installed for makeup air on the fourth and fifth floors to help achieve minimum outside air requirements.
About 25 small exhaust fans were installed in rooms with double-hung windows, and 35 supplemental fan filter units with HEPA filters were provided to recirculate air as needed. This combination of strategies helped most spaces achieve the desired number of air changes and meet (or at least approach) negative pressurization.
“There was concern our air supply was a little low, and in extreme temperatures we might struggle to maintain room temperatures,” says Mason. “But the target was to make it as good as possible. I’d say 90% of the rooms got pretty close to meeting the target value of a 100 cfm differential between supply and exhaust.”
In back-of-house and out-of-service areas, such as the prep kitchen, supply fans were run at high levels and exhausts were turned off, “just to help pressurize the building and ‘fill the balloon,'” says Mason. Locking down the connector doors between the hospital and an adjacent clinic also played a role in keeping building pressure relationships close to the targets.
Plumbing Design
According to Ficek, plumbing priorities were providing appropriate gas/vacuum services and implementing Legionella control through chlorination of the domestic hot water systems. The facility was already fully sprinklered, which removed one major issue from the plumbing/FP design.
The site includes three domestic water heater systems. “Only two of the five water heaters were working, and equipment had to be replaced,” says Ficek. “Since the facility had been shut down for months, a systemic hyperchlorination of the domestic water piping was performed, followed by verification testing to confirm that Legionella was no longer a concern. In conjunction with Earthwise Environmental, we also added a chlorine injection system to help keep Legionella at bay.”
Designed capacity for medical vacuum was apparently sufficient, but only three of the eight existing vacuum pumps were operational. “We ended up repairing two and replacing three,” says Ficek.
The hospital’s bulk oxygen tank had been removed, so there was a rush to locate a vendor who could bring in a 6,000-gallon unit. Medical air was also a concern, recalls Ficek. “They had a tiny duplex 5-hp motor compressor, and we ended up buying and installing a triplex 15-hp. We essentially went from getting 15 or 20 cfm of compressed air to 130 cfm. The typical patient rooms did not have medical air in them. Many of the rooms had to have medical air outlets added, along with local alarms.”
Because the project schedule was so short, the team decided that medical gas piping would be surface-mounted. “Many patient rooms did have medical gas outlets stubbed into them, but the pipes were inactive,” says Ficek. “And all the pipes that were stubbed were capped above hard ceilings. There was no way there would be enough time to take the ceilings down, put up pipe hangers, and get new gas supply to all the rooms, and in a lot of cases there was no space up there anyway. We ended up running the piping exposed.”
Construction and ‘Commissioning’
Getting the project built required a mix of sharp forensic skills, prompt decision-making, fast fixes, and strategic vendor relationships. For instance, addressing steam and condensate issues in the boiler plants was a hands-on proposition. “We ourselves ended up doing a lot of repair work; there was a lot of prep on systems that, in a normal job, a contractor would do for us before we tried to commission anything,” says Matsen. Long hours were spent testing equipment, troubleshooting problems, and devising spontaneous solutions.
“Every day there was a new situation and another piece of equipment that was failing,” says Villani. “There was a lot of ‘two steps forward, one step back.'”
Vander Klay adds, “John Villani and the fitters were playing steam system ‘whack-a-mole’ on component failures and leaks for three weeks.”
Says Mason, “I think there were three or four times when I had to grab scrap paper off the floor and just start sketching a design on the fly, and then handing the paper to the contractor who’d go and start building it.”
Sourcing equipment and materials was a critical task, occasionally requiring a call from an Army Corps official (or at least, the prospect of such a call) if a vendor balked at a request. Items with a typical eight-week lead time were supplied virtually overnight in several cases, including a refrigerant monitoring system and a 75-hp motor. Fan filter units for the rooms with window-based exhaust had to be shipped in batches because not enough could be located at once.
“There was always some new panic,” says Mason. “Motors would work and then they’d fail, and we’d have to send people to try to find replacements.” Villani recalls that a Nashville tornado affected the availability of some crucial equipment, but “magically, it all worked out.”
Flexible medical gas pipe was selected to provide code-required medical gas volumes, possibly for the first installation in the state of Illinois. The product, code-certified by NFPA, has not yet been approved by the Illinois Department of Public Health, but IDPH approval was not part of the emergency response facility criteria. However, project design team leaders were in contact with IDPH throughout the project, and documents were shared with IDPH for their comments and information. In addition, due to a shortage of available pipe fittings, contractors used clean, flexible copper tubing as a substitute.
Schmidt points out that, due to lack of a functioning BAS until the end of the project, when a new Honeywell controls system was finally installed, “commissioning” required putting together many partial tests to be able to say a unit or system was running as intended. “If we’d waited for steam and chilled water to work so we could test the air-handing units, we would not have had time to replace the failed valves, damper actuators, low-temperature safeties and so on that were identified. We had to adjust our approach to functional performance testing to align with the project schedule, which meant finalizing FPTs during the last hour of the day.”
Brute force, and the decision to allow exposed cabling, allowed the team of contractors to install controllers, power them, and run communication wiring to pneumatic controllers for all AHUs in a matter of a few days, says Vander Klay. “I asked a team that had just started wiring a unit when they might be done, and they said ‘by lunchtime’ — unbelievable. We were basically following up the install crews to make sure no devices were missed before we could test, and they pretty much nailed it.”
Teamwork Prevails
Beyond the unusual speed and scope of the job, team members report another rare circumstance: An extraordinary degree of cooperation, extending beyond typical roles of companies and personnel. In addition to multiple daily meetings starting at 6 a.m., impromptu communication was frequent and essential.
Recalls Matsen, “There was a running text thread with 20 or 25 participants, and for some of the phone numbers I didn’t even have names associated. But a text would come in saying, ‘We’ve got a leak in Room X, I need help.’ Three minutes later, five people would show up to help. It’s hard to describe how unusual this is. I have never been on a project where there were that many people so willing to help everyone else.”
According to Villani, the presence of the Army Corps, and the lack of a typical owner-designer-contractor decision structure, facilitated the on-time delivery. “We accomplished the mission of having it ready for patients in three weeks. It was the Army Corps’ budget to spend, and they established a clear chain of command and control of both time and money.'”
At quarter to midnight on the last day, April 24, G/BA teammates walked away from the building and met up in a remote parking lot, raising a glass to recognize a job well done.
As the uncertain trajectory of the COVID-19 pandemic unfolds, the Westlake facility has not yet been needed, and the team acknowledges that it may never be required for its intended purpose. Says Villani, “I spoke to the top Corps person assigned to the job on the last day about long-term use, and he said, ‘There are those who will second-guess decisions, but we had to make the best decisions we could with the information we had on March 20.'” Other government agencies are now considering the fate of the site (which, Villani points out, would require a good deal more work for optimal long-term functioning).
Whatever the eventual outcome, the project has left an indelible stamp on all who participated. The gravity and urgency of the work, as much as the design and construction challenges, marks Westlake as truly unique, according to Villani. “During the project, members of the project team lost loved ones to this awful pandemic,” he says. “If you want to know why we were all driven to work harder than ever before, you could see the answer in the eyes of a coworker who had just lost a loved one. I pray we won’t ever need this facility, but I am confident it will do what is needed, if and when that time comes.”
Note: This article was previously published in Engineered Systems.

To maximize occupancy, spaces originally intended to serve other functions or fewer patients were redesigned wtih a larger number of beds: All photos: Grumman/Butkus Associates

Achieving ventilation goals in some of the oldest patient rooms required HEPA-filtered fan filter units and window-mounted exhaust fans.

Many rooms had insufficient, absent, or inoperative medical gas systems. In this Level 3 patient care room, designed for the sickest patients, new oxygen, medical air, and vacuum services were provided through surface-mounted piping to accommodate the demanding schedule for completion.

Getting two separate central plants up and running was a key aspect of the renovation scope, as was supplementing the existing air-handling supply and exhaust equipment.

Robust new infrastructure was required to provide oxygen and medical air, while vacuum was supplied with a combination of existing equipment and replacement pumps.



